
Dr George Stabelos, GP, HMSA vice-president
Answers and Discussion
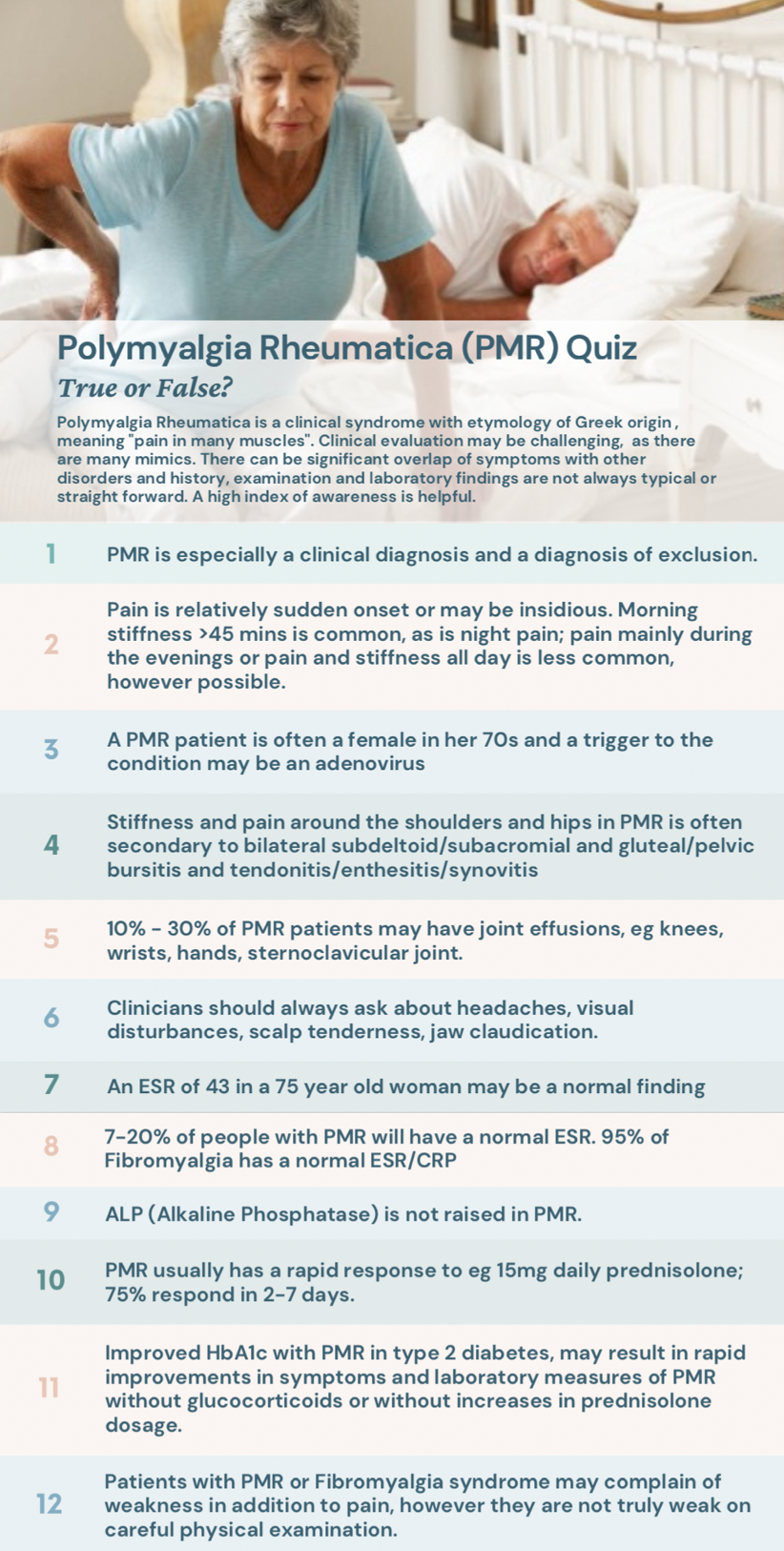
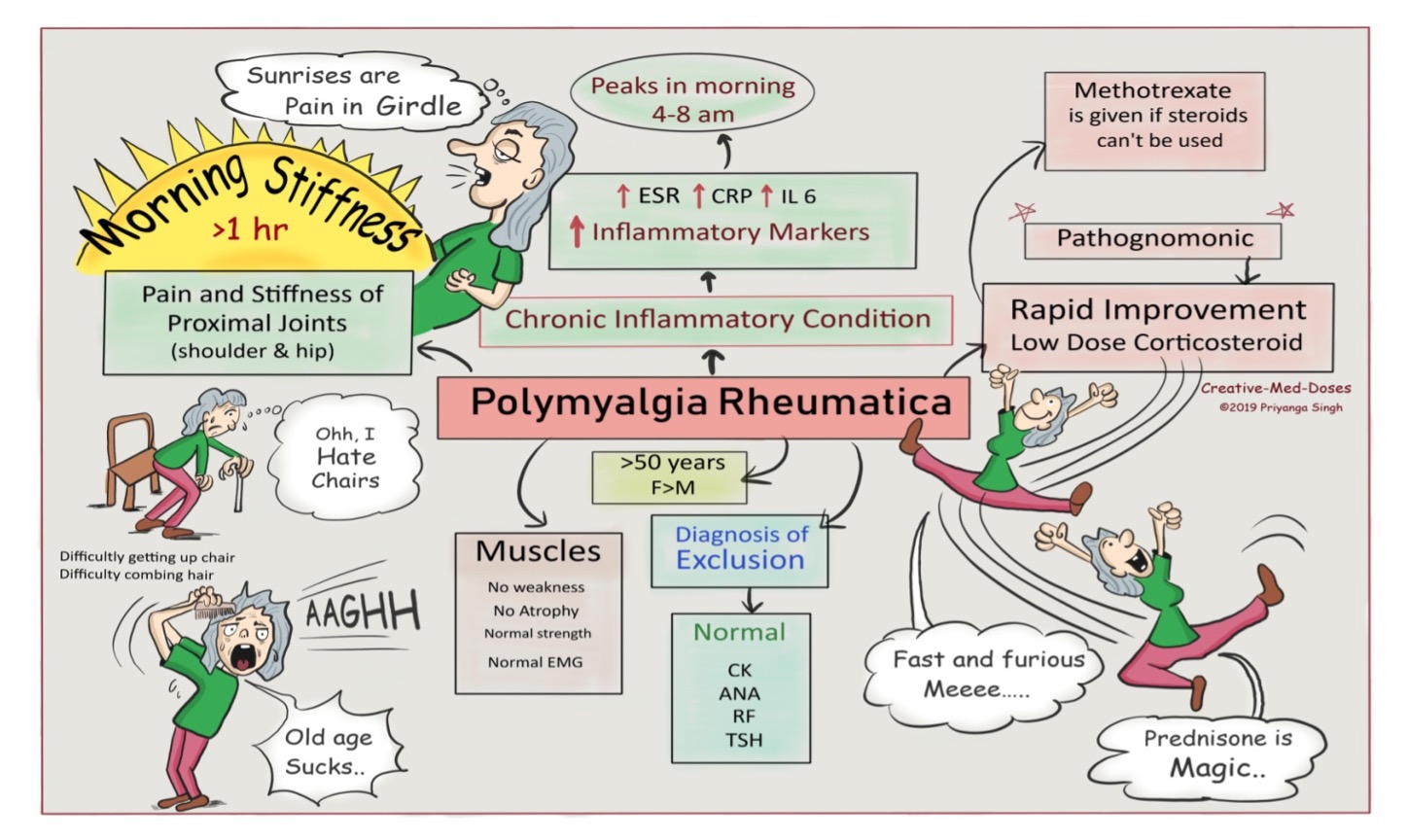
1. True. PMR has many non-specific features and a wide differential diagnosis (1). No specific biomarker, identifier or ‘gold standard’ diagnostic test is available(2), so the diagnosis is made primarily on clinical grounds, which can lead to diagnostic error. Lab findings involving eg elevation of inflammatory markers including acute phase reactants may offer supportive evidence, however are non-specific and not always reliable (see below).
2. True. Beware patients with potential Dx of PMR who do not have the typical history of morning stiffness getting better with the passage of the day. The Dx may not be the ubiquitous OA spine/shoulders/hips and/or rotator cuff or gluteal bursitis /tendinopathy!
3. True. The average age at diagnosis is > 70 years (usually >50yo), with a lifetime risk of 2.4% for women and 1.7% for men. Studies are inconclusive, however adenovirus, parvovirus B19 and parainfluenza virus are thought by some to be implicated in PMR (3-4).
4. True (6). Bursitis of the cervical interspinous bursae has also been identified, which may or may not explain neck pain (5). Fatigue, lack of appetite, weight loss, anaemia, asthenia, flu-like Sx, fever, weak feeling, are all also possible. First described by Bruce in 1888 as "senile rheumatic gout" and first termed "polymyalgia rheumatica" by Barber in 1957 in a report of 12 cases.
5. True. The DDx includes seronegative elderly onset rheumatoid arthritis (SEORA), late-onset seronegative spondyloarthropathy, SLE, myositis, vasculitis, infection, GCA, bilateral frozen shoulder, OA. Not to be missed, often without joint swelling also includes DDX: malignancy, myeloma, MDS, Parkinson's disease, thyroid disease.
6. True. 15- 20 % of PMR patients have histologic lesions consistent with temporal arteritis (8). 50 percent of people with giant cell or temporal arteritis (Κροταφική αρτηρίτιδα) also have polymyalgia rheumatica. 15% of GCA leads to permanent blindness. Tongue claudication is also a possible symptom. In GCA there is 17X the prevalence of thoracic aortic aneurysm and aortic dissection.
7. True. Rough rule of thumb for the age-adjusted upper limit of normal for ESR (mm/h) is (9): Male=age/2; Female=(age+10)/2. At 75, a normal ESR in a woman may be up to eg. 43 mm/h. ESR may exceed 100 mm/hour & may be less than 40 in a minority (5 to 20 percent) of PMR. Practice tip: always look at the baseline ESR in patients from previous years..a 75yo woman with recent ESR 43 may have PMR. ESR in GCA is almost always >50mm/hr, averaging 80-100mm/hr (Westegren)..rarely ESR may also be normal in GCA!
8. True. Some PMR patients do not have elevated inflammatory markers despite typical HX of PMR. A small % of Fibromyalgia patients have an elevated ESR, more likely if they are obese (11). Normochromic normocytic anaemia, thrombocytosis, GGT elevation is possible.
9. False. ALP is an acute-phase reactant and in a study of 74 patients with PMR it was raised in 33% of cases (12). On treatment with steroids, the ALP became normal in every case within three weeks. Some cases of malignancy may also initially respond to steroids.
10. True! Methotrexate, azathioprine may be an option in those who do not tolerate steroids or if they are not effective however evidence is unclear re benefit. Refer rheumatologist. 10-20% of PMR patients with mild disease may respond to NSAIDs/ COX2 inhibitors; beware morbidity if long term use. If you patient responds to NSAIDs, they still might have PMR, not just eg OA/ bursitis!
11. True. Improved glycaemia may reduce the prednisolone dose requirement. A Japanese case series showed significant improvement in symptoms and inflammatory markers within 2 weeks of OHA adjustment & improved glycaemia (13).
12. True. Objective examination usually shows power intact. In contrast, Polymyositis or corticosteroid myopathy on the other hand, have objective weakness with very little or no pain (in theory!). Always good to order a CK just in case! (14) In PMR, check BMD with DEXA scanning and consider calcium and vitamin D, eye check (cataracts with prednisolone) and ensure immunisations are up to date (infection risk with long term pred). Consider screen for solid organ or other neoplasia if ESR not falling with prednisolone.
Acknowledgements
A special thank you to Rheumatologist Mr Michelle Papandony for her reivew and input to this quiz and to Dr Arthur Kokkinias
References/ Links
1. https://www.racgp.org.au/afp/2014/june/polymyalgia-rheumatica/
2. http://www.rheumyearinreview.com.au/#(mediaGrid11448|popup)=https://vimeo.com/591956867;
3. https://pubmed.ncbi.nlm.nih.gov/8353986/
4. https://pubmed.ncbi.nlm.nih.gov/10948753/
5. https://pubmed.ncbi.nlm.nih.gov/18208867/
6. https://digital.library.adelaide.edu.au/dspace/bitstream/2440/116912/2/hdl_116912.pdf
7. https://www.practicalpainmanagement.com/differential-diagnosis-polymyalgia-rheumatica-rheumatoid-arthritis#:~:text=The%20most%20helpful%20distinguishing%20feature,and%20self%2Dlimited%20in%20PMR.
8. Jones JG, Hazleman BL. Prognosis and management of polymyalgia rheumatica. Ann Rheum Dis. 1981;40:1–5. cited in https://www.aafp.org/afp/2000/0815/p789.html#afp20000815p789-b14
9. Miller A, Green M, Robinson D (January 1983). "Simple rule for calculating normal erythrocyte sedimentation rate". British Medical Journal. 286 (6361): 266. doi:10.1136/bmj.286.6361.266. PMC 1546487. PMID 6402065.
10. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5911650/
11. https://emedicine.medscape.com/article/329838-workup#:~:text=While%20the%20ESR%20is%20usually,mildly%20elevated%20in%20obese%20patients.
12. https://pubmed.ncbi.nlm.nih.gov/1790639/
13. https://pubmed.ncbi.nlm.nih.gov/32926797/
14. https://ard.bmj.com/content/annrheumdis/50/5/321.full.pdf